 Want a good life? Keep clear of periodontal disease.
Want a good life? Keep clear of periodontal disease.
No kidding.
According to a study recently published in the Journal of Periodontology, gum disease can significantly lower a person’s overall quality of life. Analysis of data collected from nearly 500 individuals showed that those with poor periodontal health experienced
functional limitation, psychological discomfort, and social disability. Many had difficulty pronouncing words and experienced a decline in tasting the flavor of and eating foods.
In addition, sufferers of periodontal disease reported feeling insecure, tense, embarrassed, and irritated, often finding it difficult to relax and do normal daily activities.
Along with these negatives, of course, are the effects of the many systemic health issues associated with periodontal problems – conditions such as heart disease, diabetes, rheumatoid arthritis, stroke and lung disease.
Time and again, researchers find oral bacteria in diseased or impaired organs far beyond the mouth. Just this past week, a new study confirmed the presence of oral microbes in cases of Alzheimer’s, strengthening the suspected link between memory function and gum disease.
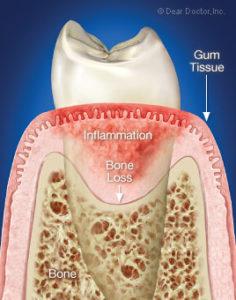 These could be classic cases of focal infection – where infection in one area travels via the circulatory system to others, spreading pathogens and other toxins that trigger secondary illnesses. But there’s another common denominator among these conditions, as well: inflammation.
These could be classic cases of focal infection – where infection in one area travels via the circulatory system to others, spreading pathogens and other toxins that trigger secondary illnesses. But there’s another common denominator among these conditions, as well: inflammation.
Inflammation itself isn’t a bad thing. In fact, it’s a normal process – your body’s response to injury or infection, in which white blood cells go to work to ward off foreign bodies or generate healing. With an external injury – a cut, say – you may notice swelling, warmth and redness. Those are all signs of the inflammatory process at work.
“Most people,” writes Dr. Mercola,
don’t realize that you need some level of inflammation in your body to stay healthy, however it’s also possible, and increasingly common, for the inflammatory response to get out of hand.
If your immune system mistakenly triggers an inflammatory response when no threat is present, it can lead to excess inflammation in your body, a condition linked to asthma, allergies, autoimmune disease, heart disease, cancer and other diseases, depending on which organs the inflammation is impacting.
When that happens, the inflammation is said to be chronic, which simply means ongoing and worsening over time. Chronic inflammation is largely fueled by lifestyle choices: diet, in/activity, tobacco and other drug use and so on. Make better, more healthful choices and you lower your risk of disease immensely. You’re no longer adding fuel to the fire, so to speak.
Periodontal disease, too, is largely lifestyle-driven, though one risk factor trumps all others: smoking. It’s practically a guarantee of gum disease. Nutrition and hygiene also play major roles, but other risk factors may not be so obvious: chronic stress, heavy alcohol consumption and lack of sleep.
Interestingly, a 2007 Journal of Periodontology study found that lack of sleep was the second most significant risk factor in the progression of gum disease.
Science continues to shed light on the interrelatedness of inflammatory conditions. Last month, for instance, the British Dental Journal published a paper theorizing “a triangular relationship” between three such conditions: obesity, diabetes and periodontal disease. Each, suggests the author, likely contributes to the others. It’s not a simple matter of cause and effect but a dynamic that generates health problems at numerous sites.
While it is accepted that both type 1 and type 2 diabetes are major risk factors for the development and progression of periodontal disease, there is growing evidence that obesity is both an indirect risk factor because it affects glycaemic control and a direct risk factor because secretion of pro-inflammatory agents by adipose tissue modifies the periodontal reaction to the plaque biofilm. Recent research suggests that periodontitis may adversely affect glycaemic control, which can be improved by periodontal treatment with reduced risk of diabetic co-morbidity, thereby creating a two-way relationship. Furthermore it appears possible that periodontitis may stimulate inflammatory change in adipose tissue, creating a triangular self-generating cycle of morbidity linking obesity, diabetes and periodontal disease.
Around the same time, another paper appeared on the association of erectile dysfunction with chronic gum disease.
The results in the present study suggest that ED is related to the damage caused by endothelial dysfunction and the systematic inflammatory changes associated with CPD. The present study also suggests that dental health is important as a preventive medicine for ED.
And, we might add, for all manner of other inflammatory conditions. This should be no surprise. Mouth and body are not separate entities. The mouth is part of the whole – and the whole is attached to the part. Once you recognize this, you find how odd it is to ever think that one part could be affected without having any impact on the rest of the whole – as if you could pour a bit of salt into a glass of water and have only one part of the water turn to saline.
Good oral health is the foundation of good overall health. And vice versa.
Inflammation image via Dear Doctor