Say you visit a doctor for a routine check-up. You have no complaints: no pain, no problems. But the doctor says, “You know, I think we’d better remove your appendix.”
“Why?” you ask.
“It might get inflamed or infected someday, at which point we’d have to do an appendectomy anyway. Besides, you don’t really need it. So I think we should remove it now, just to be on the safe side. It’s preventive medicine!”
Of course this is a ludicrous scenario. And yet many dentists – doctors of the teeth and other oral tissues – make this same sort of justification when it comes to the removal of non-impacted wisdom teeth (“hedge” words in bold for emphasis):
First, an impacted wisdom tooth may accumulate food debris around the gums creating a breeding ground for bacteria. Once bacteria present, the wisdom tooth might decay or worse, the tooth next to it may decay too. If not treated early, this tooth decay may eventually lead to an infection.
From here, it’s one step to the slippery slope of all the bad things that result if the above conditions are met and not properly treated: halitosis (bad breath), caries (cavities), periodontal (gum) disease, infection and necrosis (bone and tissue death).
 But these outcomes are probable when any teeth aren’t taken care of properly – not just wisdom teeth. So advocates of wisdom tooth removal for all have an additional justification at the ready: wisdom teeth, they insist, are really, really, really hard to clean. And since they’re really, really, really hard to clean, they will be that breeding ground for microbes and thus at risk for caries and and so on. Besides, they say, no one really needs their wisdom teeth.
But these outcomes are probable when any teeth aren’t taken care of properly – not just wisdom teeth. So advocates of wisdom tooth removal for all have an additional justification at the ready: wisdom teeth, they insist, are really, really, really hard to clean. And since they’re really, really, really hard to clean, they will be that breeding ground for microbes and thus at risk for caries and and so on. Besides, they say, no one really needs their wisdom teeth.
Now, if you consider them from a purely functional standpoint, sure, we can get along just fine without wisdom teeth. But teeth are more than mere “gnashers.” They are vital, living organs within and connected to the body as a whole. Unlike what happens in Vegas, what happens in the mouth doesn’t always stay in the mouth, as we see when, for instance, the microbes involved with periodontal disease show up in the diseased heart.
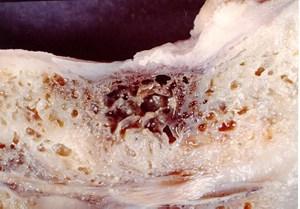
One of the problems with unnecessary medical procedures is that they subject the body to trauma it would not experience otherwise, thus increasing health risks. A major risk of extraction is the formation of cavitations – especially when the surgeon fails to clean out the socket thoroughly and completely remove the periodontal ligament that attaches the tooth to the underlying bone. In simplest terms, a cavitation is a hole in the jawbone surrounded by dead and decaying tissue. As such, it becomes a harbor for microbes and their metabolic byproducts: toxins which ultimately enter the body’s circulation and thus pollute the terrain, infest other organs and can give rise to systemic illness and disease. While cavitations may be caused by any number of things – severe periodontal disease, cysts and the effect of toxic dental materials, for instance – the most common cause is tooth extraction. And it’s worth noting that an estimated 45% of all cavitations occur at the wisdom tooth sites.
 Now, do all extractions lead inevitably to cavitations? Of course not. So it could be argued that we, too, are arguing on the basis of “might.” However, where an individual can minimize risk of infection through proper dental hygiene, there is no analogous action to prevent cavitations. If they result from the surgery, the only solution is more surgery, plus the necessary detoxification and restoration of the biological terrain (the body’s internal environment). Moreover, decay can be caught and treated early. Cavitations are usually discovered only well into the disease process, where the individual has already grown quite sick from the toxication of the body.
Now, do all extractions lead inevitably to cavitations? Of course not. So it could be argued that we, too, are arguing on the basis of “might.” However, where an individual can minimize risk of infection through proper dental hygiene, there is no analogous action to prevent cavitations. If they result from the surgery, the only solution is more surgery, plus the necessary detoxification and restoration of the biological terrain (the body’s internal environment). Moreover, decay can be caught and treated early. Cavitations are usually discovered only well into the disease process, where the individual has already grown quite sick from the toxication of the body.
In sum, the health risks are greater, especially in cases where the teeth are causing no problems.
Of course there are times when removal of the wisdom teeth may be appropriate, such as when they are impacted (wedged against the second molars and unable to erupt properly). But to say that everyone should have their wisdom teeth removed because they might cause problems is not, in our opinion, wise dentistry. As with appendices – and tonsils, as well – there is simply no good reason to remove healthy, functioning organs from a body on the basis of “might.”
And indeed, over the past few years, more research has been published, showing that third molar extraction is often unnecessary:
Teens often have their wisdom teeth removed. But there’s no evidence this painful procedure prevents future trouble.
That’s the conclusion of a careful review of dental studies by a research team including Dirk G. Mettes, DMD, of Radboud University Medical Center in, Nijmegen, Netherlands. Although Mettes and colleagues looked at 40 studies, they found only two controlled clinical trials of wisdom tooth removal.
The bottom line: If impacted wisdom teeth are not causing trouble, there’s no evidence that removing them helps or hurts future health. But there is some evidence that removing teens’ impacted wisdom teeth “to reduce or prevent late incisor crowding cannot be justified,” the researchers conclude.
The abstract of the study mentioned is available here.
Consequently, the American Public Health Association has released a policy paper (PDF) in which they recommend against routine removal of wisdom teeth, showing that – and how – the justifications for such removal simply do not stand up to scrutiny.
The main arguments for prophylactic removal of third molars are: unpredictability of eruption; damage to adjacent teeth; harboring of pathogenic bacteria that may cause periodontal disease and may contribute to low infant birthweight and other diseases such as diabetes, cardiovascular disease and stroke; may cause crowded or crooked teeth; easier to extract and less morbidity when extracted in adolescence.
None of these contentions are sufficient to support prophylactic extraction of third molars. Unpredictability of eruption is not valid because most wisdom teeth erupt and only a small percentage of those that remain unerupted or partially erupted cause problems that warrant extraction. All periodontically diseased teeth harbor pathogenic bacteria and require treatment by general dentists, dental hygienists and periodontists, whose goal is to retain, not extract, them. Presence of third molars in conjunction with systemic diseases represents association, not causation.
The paper goes on to review the scientific literature informing the organization of its position on the matter. And though the label “policy paper” sounds deadly dull, we know, this one is really worth a read – especially by those who have been told by their dentists that they need their wisdom teeth removed even though those teeth are causing no problems.
Being a statement from an organization concerned with matters of public health, the paper situates itself within the issue of the American habit of overspending on health, particularly in the name of “prevention” (as we have discussed previously):
Excessive health care in the United States has been documented by numerous studies. It results in waste of limited funds and harm to millions of people, not excluding death, because even the safest treatment is not without risk. The obvious solution, when effectively applied, is “evidence-based practice,” which minimizes unnecessary procedures and reduces costs. The public is already aware that some surgical procedures such as tonsillectomy are no longer routinely performed in the absence of infection to prevent future infection. Yet, there are procedures such as the prophylactic removal of third molars that result in injury to tens of thousands of people at a cost of billions of dollars, about which the public is ill informed and thus subject to the risks of unnecessary surgery.
Let this be one small step toward helping “the public” become better informed.
Originally published on Know Thy Health, by the office of Gary M. Verigin, DDS, CTN. Used with permission.